Inflammatory Bowel Disease (IBD) vs Inflammatory Bowel Syndrome (IBS)
IBD-AID Phases, Diet, Gut dysbiosis, Fiber for IBD, Nutrition Interventions, Low FODMAP Diet
IBD
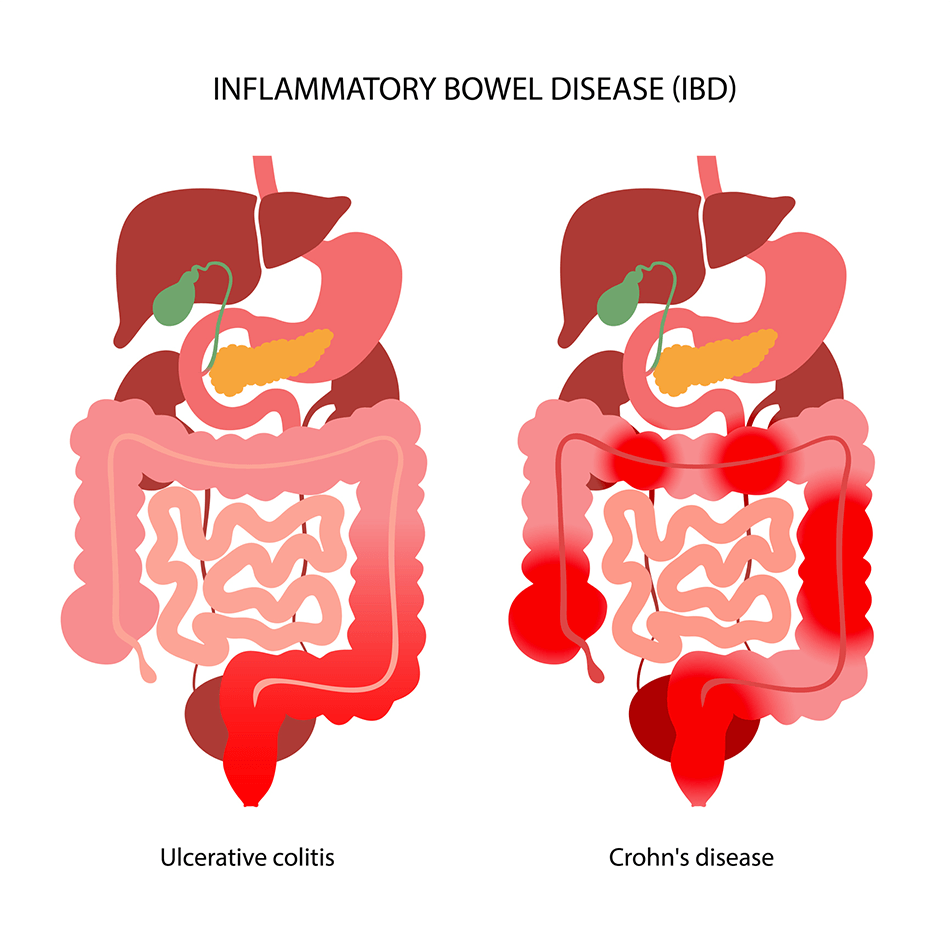
A term for 2 conditions: Crohn's Disease and Ulcerative Colitis. It is a chronic inflammatory condition.
IBS
A group of symptoms that occur synergistically: consistent pain in the abdomen and changes in bowel movements including diarrhea, constipation, or both. Unlike IBD, in IBS you have these symptoms without any visible signs of damage or disease in your digestive tract.
Introduction
If you go to a medical doctor and get prescribed steroids, and they fail as they most often do, then the next option is a biologic. When you take a biologic it comes with a host of side effects:
Biologic induced lupus or arthritis (widespread joint pain)
The safe(r) option is to explore the nutritional options before a biologic or surgery. There are 3 pillars with IBD, and they all are interact with one another:
Dysfunctional immune system
Chronic inflammation
Disruptive microbiome
One could use supplements to fix the microbiome, but it’s usually not enough to get to the root issue. The problem with just fixing the microbiome with probiotics or antibiotics or prebiotics or other bacterial species is that it may not be the only thing that is involved in the microbiome. Certain foods help feed good bacteria to create short chain fatty acids, which strengthens the mucosa layer and thus reducing intestinal permeability and reducing inflammatory response.
Butyrate is a short chain fatty acid that is produced when the good bacteria in your gut helps to break down the dietary fiber in the large intestine; butyrate directly impacts the immune system by increasing T regulatory cells in the gut. The T regulatory cells are the one cell(s) that apparently tell the body to not attack itself, and to gain immunotolerance.
Fiber
Over time you want to eat more fiber, but slowly incorporate it into your diet. There are 2 types of fiber: soluble fermentable fiber and insoluble non fermentable fiber. The main component you want to know is whether the food is fermentable or not, which means can the gut bacteria use the fiber for energy? If it non fermentable that means you and your gut bacteria can’t use the fiber for energy…it goes right through you. Those non fermentable fibers are known to induce a flare up…so avoid non fermentable insoluble fiber. An example of these non fermentable insoluble fiber are broccoli stems or a raw vegetable diet. Raw vegetables have.a specific fiber in it called cellulose, which is non fermentable and does not improve the microbiome and with colon inflammation it can induce a flare up
Soluble fermentable fibers are typically softer and digest easier. An example is steel cut oats, which contains polyphenols and nutrients which will help improve the microbiome, and it is unrefined. Steel cut oats are better than eating for example white rice which is deprived of minerals and vitamins. White rice may help with the current flare up, but long term you’re not improving your microbiome. Whereas with Steel cut oats, cooked well and mushy, has a great source of fiber- has per serving roughly 1.7mg of iron, .2 mg thiamin, 40 mg magnesium, 20 mg calcium, 170 mg potassium, and 190 mg phosphorus.
Another good source is psyllium husk which has a lot of research behind it with IBD. see paragraph below. The only caution is to start small and increase it if you respond well. You can start with 5 grams/week and increase it slowly week to week.
So if you are avoiding fiber and have IBD, know that there are different types of fiber. Psyllium husk may be a good option. Over time you want to increase your fiber to 20-40 grams of fiber/day.
Two studies by Hallert et al. and Fernandez-Banares et al. found an overall benefit in patients with inactive UC from consuming psyllium husk or seeds [33,71]. The first RCT of a four month duration found that consumption of psyllium husk improved gastrointestinal symptoms in these patients [33]. Questionnaire-based scoring of abdominal pain, diarrhoea, loose stools, urgency, bloating incomplete evacuation, mucus and constipation had improved compared to baseline. However, the 13 patients in the placebo-group also showed minor improvements, possibly because crushed crispbread that contained 17.3% of insoluble DF was given. This suggests that both supplements of psyllium husk and the “placebo” could provide benefits in reducing symptoms commonly experienced by patients. The other open-labelled RCT of 12-months duration compared the intake of psyllium seeds with or without mesalamine treatment to a control group [71]. Mesalamine is a 5-amino-salicylate with general anti-inflammatory effects, often used as front-line therapy in UC [72]. Results of this combination showed that the treatment failure rate was 40% in the psyllium group, 35% in the mesalamine group and 30% in the group taking psyllium and mesalamine together. However, these differences were not statistically significant, and the probability of continued remission was similar in all three groups. Furthermore, patients consuming psyllium seeds had increased faecal levels of butyrate, which the authors linked to the maintenance of disease remission.
Wong C, Harris PJ, Ferguson LR. Potential Benefits of Dietary Fibre Intervention in Inflammatory Bowel Disease. Int J Mol Sci. 2016 Jun 14;17(6):919. doi: 10.3390/ijms17060919. PMID: 27314323; PMCID: PMC4926452.
Chrons vs Ulcerative colitis
Fats are the only nutrient absorbed in the colon; protein and carbohydrates are absorbed in the small intestine. Fats have to get mixed with bile and be transferred into the colon so if you have colon inflammation, you have to be careful of the types of fat you’re consuming. There is a lot of research that is clear on this that long chain saturated fats like in butter cause more of a flare up.
Chrons disease is a full GI tract issue but can be only in the colon, that can range from the rectum to mouth or lips, and esophagus inflammation causing acid reflux. Thus chrons affects the entire mucosa layer. The signature finding for chrons is pathognomonic, if your doctor does a colonoscopy and find skip lesions then you have chrons, which means there is damage tissue in the colon separated by healthy tissue separated by damage tissue. See photo below.
Both chrons and UC you need a colonoscopy to confirm.
Ulcerative colitis is continuous inflammation without skip lesions and only contained in the colon not the entire GI tract, and contained in the inner most mucosa layer.
If getting blood work, it will reflect the following as high as inflammation may be present:
High C-Reactive Protein or high ESR (erthrocyte sedimentation rate) biomarker are the inflammatory markers and
increased TNF, interleukin 17, and interleukin-1 beta
Food suggestions/ Diet strategy
The worst protein to consume for IBD is red meat because of the heme in the meat that contains the iron when it goes down to the colon if there is existing oxidative stress in the colon then the iron promotes the inflammation. Leaner white meat, chicken, turkey, fish, and dairy (lactose free milk works), eggs ; all are better than red meat
Fats : flaxseed oil is your best option, avoid vegetable oil, avoid long chain saturated fats (butter and animal fats), medium chain fatty acids acids are good because they’re not absorbed in the colon only in the stomach and small intestine….so MCT oil or unrefined coconut oil both can work well. Choose olive oil instead of canola oil - both have monounsaturated fats and have the same fatty acid profile but extra virgin olive oil has anti inflammatory polyphenols. Avoid vegetable oil.
Carbs: steel cut oats, rolled oats seem to have a good reputation. The most important for carbs for IBD is texture…making the foods more mushy may be easier to handle….or puree the foods to avoid the flare ups. Most fruits are OK, but bananas, papaya, and apples work well, but with Apples the skin can act as a flare up so it should be peeled.
IBD-Aid Nutrition Protocol
I went over the IBD-Aid Nutrition Protocol and more information can be found here https://www.umassmed.edu/nutrition/ibd/ibd-aid-phases/. There are 3 phases with this protcol:
Phase 1 current flare up
Phase 2 intermediate symptoms
Phase 3 remission
Low FODMAP Diet
More information on that can be found here: https://www.health.harvard.edu/diseases-and-conditions/a-new-diet-to-manage-irritable-bowel-syndrome
Great for IBS
Low FODMAP does not have experimental research that it improves IBD over time
Low FODMAP diet restricts fiber, you want to keep the diet to improve your microbiome
Flaxseed oil, Curcumin, Omega-3
Omega 3 is tricky and there is a lot of information about it. Omega 3 is anti inflammatory (fish oil). The clinical trials of IBD suggest that use fish oil show no results for IBD…why? It’s not just the omega 3 that is important, it’s the ratio of omega 3 to omega 6. Keep in mind one should limit going out to eat too often as it is loaded with vegetable oil, which is loaded with omega 6.
Flaxseed oil, one of several studies https://jpma.org.pk/PdfDownload/11027 discuss rheumatoid arthritis, and how flaxseed oil beat fish oil in RA patients.
There is something called oxylipids, these are oxidized metabolites that are produced from both flaxseed and fish oil. The type of fat in flaxseed oil produces its own independent anti inflammatory oxylipids that fish oil can not produced. The research that is coming out sho that flaxseed oil is beating fish oil in autoimmune conditions such as MS, psoriasis, Rheumatoid arthritis.
The benefit of flaxseed oil is you dont have to keep it at the same dose as fish oil. Fish oil can become unsafe if consumed in high amounts such as above 12 grams fish oil per day. Fish oil is a long chain fatty acids and has the most amount of double bonds, which means it is higher probability of being oxidized in the body.
I have made several videos about turmeric, and use it extensively. I would extend this gesture to you to begin incorporating it into your diet. There is a line of research that taking turmeric/curcumin as a supplement may elevate the enzymes in the liver that convert the flaxseed fatty acid to fish oil fatty acid
Conclusion
Avoid vegetable oils and no eating out more than 2x/week. Veg oils can be found in a lot of foods - even “healthy” cereals
Supplement with flaxseed oil - 1 tbsp/day